Exercise Rehab for Elders Recovering from a COVID-19 Diagnoses
Posted on:

Times are tough; there is no doubt about it. For most of us, the world that we know will never be the same because of the pandemic that is, COVID-19 (COVID). I am in my mid-30s, and never have I recalled a time when something as invasive and life-altering has affected me. There are millions, if not billions of people that can say the same thing. The purpose of the article that you are about to read is to educate on what COVID is, explain the epidemiology behind the virus, and provide rehabilitative recommendations on how to successfully rehab geriatric persons recovering from a COVID diagnoses.
According to the CDC, COVID belongs to a family of viruses called Coronaviruses, which are known to cause illness responsible for the common cold and more serious diseases such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). In a recent interview on CNBC, the U.S. Director of the National Institute of Allergy and Infectious Diseases, Dr. Anthony Fauci, reported that the virus is “very different,” from what we have observed with other outbreaks. What makes COVID different from anything experienced by past generations is that the virus was transmitted from an animal host. The COVID outbreak and first reported transmission from animal to human originated in Wuhan province, China in December of 2019.
What makes COVID so dangerous is the high potential for person to person transmission through infectious particles. Airborne droplet particles can remain suspended in the air for long periods of time, and once having settled on a solid surface, can remain alive for even longer. According to a new publication from the New England Journal of Medicine, coronavirus can be found for up to 3 hours in the air, 24 hours on cardboard, and 2-3 days on plastic and stainless-steel surfaces. The best way to combat the risk of transmission and spreading of the coronavirus is to develop a strict, routine schedule for sanitization and cleaning of all surfaces that the ordinary person may encounter.

The epidemiology for any health event or infectious disease is defined by the Centers for Disease Control & Prevention (CDC) as, “the study of the distribution determinants of health-related states and events in specified populations.” The coronavirus, more specifically COVID, is classified as a zoonotic virus, meaning it is found in animals as well as humans. Infected individuals can be either symptomatic or asymptomatic, with symptoms ranging in severity from minor illness to the need for hospitalization. The chart listed below shows symptoms associated with coronaviruses as in comparison to the common cold and flu symptoms.
The pathogenesis (manner of development of a disease) of COVID starts with the binding of the virus to oxygen receptors on returning red blood cells (RBCs) in the lungs. This effectively blocks the potential for re-oxygenation of those RBCs during the 02-C02 exchange. Dr. Yehuda Shoenfeld, physician, and autoimmune researcher from the Hebrew University of Jerusalem suggests that symptoms of COVID, “are similar to that of hyperferritinemia.” Hyperferritinemia (HFE) is the build-up of iron storage proteins called ferritin in the blood and cardiovascular system. Ferritin is very important for the human body because it assists with cellular oxygen metabolism, but, in large quantities, can be harmful. De-oxygenated RBCs returning to the lungs are already carrying ferritin to assist with converting oxygen into useable energy for viable tissue. When the 02-C02 exchange occurs in a host positive for COVID, instead of getting a nice oxygen molecule, oxygen receptors on the RBC are blocked and replaced by the virus. Because there is no longer a need for ferritin, the RBC releases this protein into the bloodstream. If too much iron is released into the bloodstream, it can lead to hemochromatosis, adversely affecting the body’s Hepatic and Renal function (liver and kidney), leading to multi-organ failure in severe cases.
What makes COVID-19 a, “Novel,” virus is that it is a product of nature versus human engineering, as some conspiracy sources have reported. Scientists from the Scripps Research Institute have found that there is, “…no proof that it is a product of bio-engineering in laboratory facilities by conducting a comparative analysis of genomic data.” When a host is infected, the virus will move down the respiratory tract to pair with ACE-2 receptors. ACE- 2 receptors are proteins on the outside of specialized cells and can be found throughout the lungs with larger and more localized amounts of these proteins in the lower lungs. Due to a more substantial presence of ACE-2 receptors in the lower lungs, the coronavirus penetrates far deeper into the respiratory tract than other viruses, such as the common cold. Once the coronavirus has been transferred to the host, it can take approximately 2-14 days before symptoms are realized. According to the World Health Organization (WHO), more than 100,000 new cases are being reported each day worldwide.
Coronaviruses are especially concerning because there is the very real potential for further exacerbating or complicating underlying chronic and acute conditions. Pleuritis (inflammation of the lungs) is a common symptom of coronaviruses, making it difficult to breathe and interferes with oxygen-carbon dioxide exchange (02-C02 exchange) that occurs within the alveoli. With pleuritis comes the potential for fluid retention and pooling in the lower lungs. If it is not caught early enough, it may develop into pneumonia, further complicating a host’s medical condition. Those with immunosuppressive or blood born illnesses such as Anemia (Anemia indicates a low red blood cell count) are going to be at a much higher level of risk. Someone with a diagnoses of chronic obstructive pulmonary disease (COPD) or a relating chronic respiratory condition is also going to be at a higher level of risk for severe symptoms due to already compromised 02-C02 exchange. Most of these people may already be on supplemental oxygen and already demonstrate with fatigue due to a decline in their blood-oxygen saturation level (02 sat level) with minimal to moderate activity.
After learning a little more about the epidemiology of COVID, it only stands to reason that certain populations are going to be more susceptible to adverse and severe reactions. The following chart represents the most recent data collected by the CDC as it pertains to age groups most affected by COVID. The Number’s section along the vertical axis represents as per 10,000 cases and breaks down the number of hospitalizations, ICU admissions, and reported deaths for each age group.
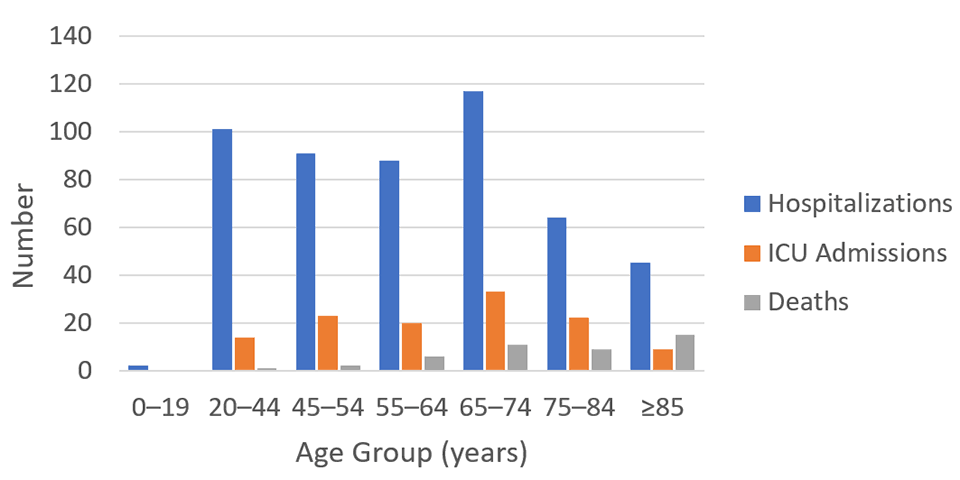
https://www.cdc.gov/coronavirus/2019-ncov/images/chart-higher-risk-older-adults.png
As you can see from the collected data, persons of 65-74 years of age are most affected with increased hospitalizations and ICU admissions. Deaths associated with the coronavirus are much higher for those of 65 years of age and older. The reason for this can be partially attributed to the aging process. As we age, our body systems become slower to respond and may even become compromised. Lifestyle choices, stress, and physical activity all contribute to how fast our bodies age and how we combat infectious diseases. People of 65 and older are also going to be more prone to having an underlying chronic medical condition versus younger age groups. These are all examples and reasons as to why COVID can be more serious in Elder populations.
For an Elder recovering from a COVID-19 diagnoses, the recovery is more than likely not going to be immediate. The length of time for recovery will depend largely on the severity of symptoms, previous medical conditions, and functional level prior to having contracted the coronavirus. The primary care physician may decide that skilled Physical and Occupational Therapy services may be necessary to address deficits including but not limited to:
- Functional endurance.
- Generalized weakness due to a decline in fine and gross muscle strength.
- Increased difficulty with performing activities of daily living (ADLs).
- Difficulty with walking and unsafe gait, largely due to generalized weakness.
- Balance deficits that may become more apparent due to inactivity or being bedridden due to the coronavirus.
I cannot emphasize enough; how crucial it is to make sure to follow isolation and personal protective equipment (PPE) recommendations during treatment. When in doubt, check with your immediate supervisor, human resources, or compliance representative. Always be mindful of vitals (blood pressure, heart rate, 02 sat levels, and respiration rate). Take them frequently throughout treatment to monitor changes and tolerance to varying levels of physical activity. Movement and activity are important throughout the disease process to promote circulation, maintain muscle length, and prevent exacerbation of symptoms or condition.
The musculoskeletal assessment in the Therapist’s plan of care (POC) should be the basis for which to establish a current level of function to use as a comparison to the previous level of function. When testing for muscle strength, make sure to test both type I (slow-twitch), and type II (fast-twitch) muscle fibers. Sometimes when testing for strength, it can be very easy to be deceived or get inaccurate data. The initial resistance applied to a muscle during manual muscle testing will give an accurate reading of the strength of fast-twitch muscle fibers. But sustained resistance of approximately 2-4 seconds during testing of a muscle group can result in the patient breaking testing position, indicating weakness in slow-twitch muscle fibers. It is important to discern the difference between initial versus sustained muscle strength and document accordingly.
When deciding on specialized testing to provide objective measurements on endurance, the 6 Minute Walk Test (6MWT) can be effective in measuring aerobic ability and functional tolerance. To perform the test, you will need a
- 30-meter stretch of unimpeded walkway.
- Stop-watch to initiate and conclude test.
- Two cones to serve as turning points at either end of the track.
- Pulse oximeter: to measure heart rate and blood 02 sat levels. Patient should be aware throughout entirety of test.
- Rolling foot/distance counter.
During the test, should the patient become fatigued, they can stop and rest against a wall and then commence with walking until the 6 minutes is up. While monitoring 02 sat levels, should the patient’s 02 sats decrease below 90% immediately cease activity, and keep note of the amount of time for 02 sat levels to return to baseline value before commencing with test. Do not stop the clock. Make sure to document total amount of feet covered within the period of 6minutes, patient tolerance, and observations during gait.
Therapeutic exercise should be geared towards high repetitions and low intensity to assist with building endurance through emphasis on slow-twitch muscle fiber activation. A really good way to show progress with improvements in strength and activity tolerance is to instruct the patient to perform a particular exercise for as many as reps as they can in one minute. Make sure that repetitions are documented and kept track of for each exercise provided. Progression can be tracked and shown through improved tolerance and increased repetitions.
Graded therapeutic exercise and physical activity are always encouraged when recovering from a COVID-19 diagnoses. At this time, there are currently 100 coronavirus vaccines being studied around the world. Twelve of those vaccines are currently undergoing human trials. Social distancing, sanitization of surfaces, and donning of an N95 mask when in public places are some of the best ways to keep our Elders safe.

